(BPT) - Liza Bobrow didn't think it was a big deal when her handwriting suddenly went haywire.
"It was just so bizarre," she remembers. "My handwriting was getting teeny-tiny. I couldn't even sign a check. I had just turned 50 so I thought 'I'm getting old. I must have arthritis, or a pinched nerve or writer's cramp.' So, when the doctors told me it was Parkinson's Disease, I was terrified."
Medication helped at first.
Her handwriting returned to near normal. But Parkinson's is a progressive disease - it usually worsens over time.
Two years after her diagnosis, the medication began triggering bouts of dystonia. She suffered painful muscle spasms in her feet that made walking difficult. Her right arm would suddenly shoot out and she would have to cradle it back in with her left arm.
"The pain was so bad that I didn't want to take the medication," she said. "But without the medicine I struggled with motor skills. It was a terrible time."
Neurologists eventually suggested deep brain stimulation (DBS), a surgical procedure in which electrodes are implanted in specific spots in the brain to deliver electrical stimulation to help control tremor, rigidity, and bradykinesia. Bobrow and her husband spent six months researching DBS and consulting her doctors before deciding to proceed.
"I had never had surgery in my life, so the idea of brain surgery was pretty scary," she said. "But I had an incredible experience, and the results are profound. My motor skill fluctuation is less and in general it's just a feeling of relaxation and comfort in my body that I just didn't have before DBS."
Liza's story is based on her individual experience. Not all patients will experience similar results.
Revolutionary leap in DBS therapy
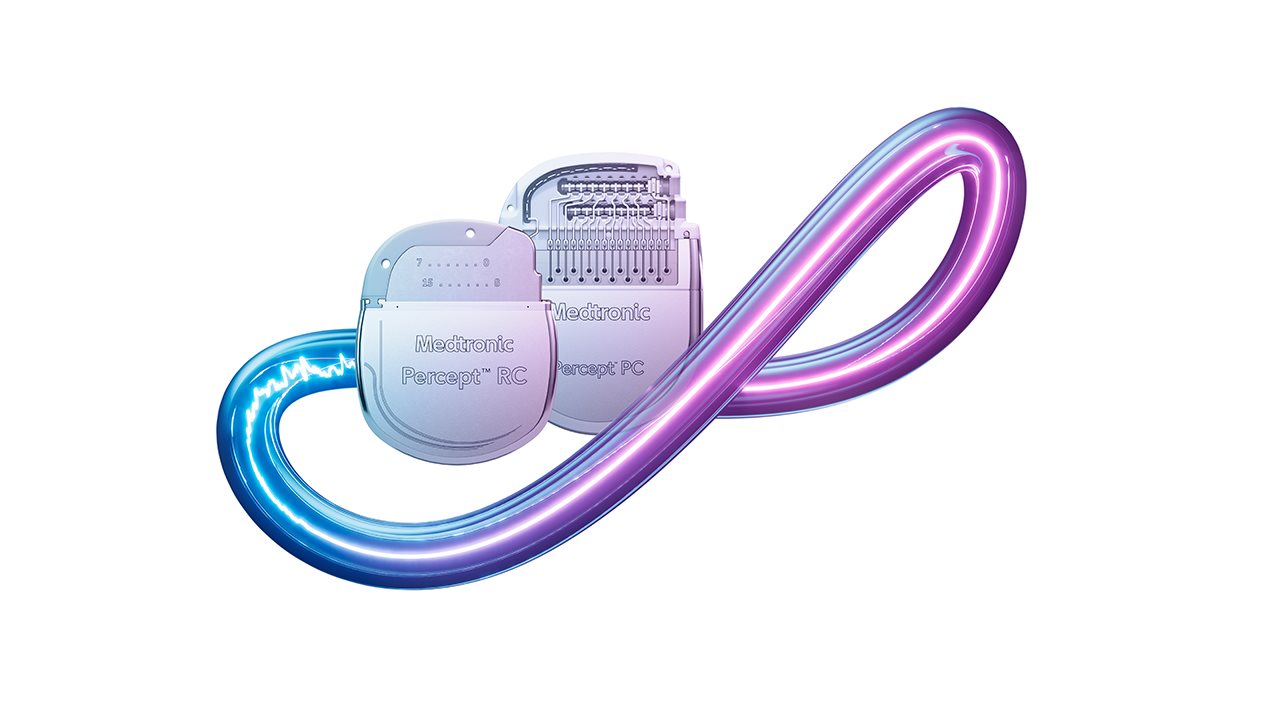
DBS has been around for decades. A pacemaker-like device is implanted in the upper chest and thin wires lead to precise locations in the brain, where electrodes deliver electrical stimulation that can help control some of the symptoms from Parkinson's.
Even though traditional DBS is proven as a safe and effective treatment for Parkinson's, the level of stimulation is constant/pre-programmed. But it has limitations. The human body and brain are constantly changing and adjusting, as the various symptoms of Parkinson's disease and medication levels can fluctuate in intensity throughout the day. So, the amount of electrical stimulation needed to optimally treat Parkinson's may also change.
"I went through a lot of programming sessions to refine the device settings," Bobrow said. "You can't just set it and forget about it."
For many patients, that's about to change.
The United States Food and Drug Administration (FDA) recently approved the Medtronic Adaptive Deep Brain Stimulation (aDBS) system for use in the U.S. for patients with Parkinson's disease. With aDBS, the electrodes that deliver electrical stimulation can also sense the patient's brain signals and automatically adjust the level of stimulation to meet the patient's needs.1 A few programming adjustment visits may be needed in the first few months after turning on Adaptive Therapy. Patients programmed with Adaptive Therapy may require more programming adjustment visits if they experience stimulation-related side effects or need to further personalize programming settings.
"The aDBS system listens to these brain waves, and then algorithms adjust the stimulation in real time according to what the brain waves tell us about their symptoms. It's a very exciting development," said Dr. Simon Little, a neurologist at the University of California San Francisco (UCSF).
As with traditional DBS, there are risks and benefits of aDBS. Risks of DBS may include surgical complications, infection, failure to deliver therapy as needed and/or worsening of some symptoms. Talk to your doctor about your medical condition and the risks and benefits of this therapy. A prescription is required, only your doctor can determine whether this therapy is right for you.
Living the dream
Liza Bobrow received her DBS device before the FDA approval of aDBS; however, a software upgrade to aDBS does not require surgery. Her device already includes the brain-sensing technology†; if her doctors decide she is a candidate for aDBS, it would be a matter of activating this technology in her current device.
"Adaptability is obviously the next frontier. I can tell that my body has ebbs and flows, and clearly real-time stimulation adjustment is something that interests me," Liza said.
Dr. Philip Starr, professor of neurological surgery at UCSF, adds: "So the dream of these brain pacemakers, which is really what they are, is to go that route and understand brain signals - and how they relate to specific signs and symptoms of movement disorders or other disorders - to understand those signals well enough to use them to auto-adjust stimulator levels. So adaptive deep brain stimulation is really synonymous with closed-loop stimulation."
Brief Statement: https://www.medtronic.com/en-us/l/patients/treatments-therapies/deep-brain-stimulation-parkinsons-disease/important-safety-information.html
† The sensing feature of the Percept™ PC and Percept™ RC system is intended for use in patients receiving DBS where chronically recorded bioelectric data may provide useful, objective information regarding patient clinical status.
References:
- Stanslaski S, Summers RLS, Tonder L, et al. Sensing data and methodology from the Adaptive DBS Algorithm for Personalized Therapy in Parkinson's Disease (ADAPT-PD) clinical trial. NPJ Parkinsons Dis. 2024;10(1):174.





